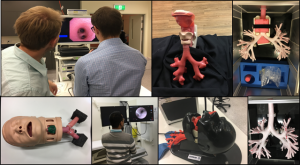
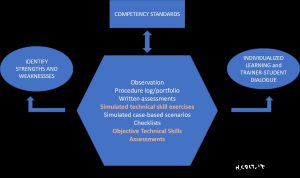
Less than 24 hours after leaving the WABIP World Congress in Rochester Minnesota, I spent a day climbing to a wonderful spot high above a bed of clouds in Southern California. An open horizon, blue skies and a soft wind caressed my face as I stood virtually alone on a rocky peak. Pausing just long enough for a protein bar, a swig of water and a photograph, my thoughts wandered for a moment back to the events of our international medical meeting. With almost 9000 members representing more than 55 different national medical associations, the WABIP has truly become an international medical society. New scholarship programs and visiting professor travel grants target leaders in developing countries, an expanding WABIP Newsletter reaches out to more than 4000 members who consistently open and read the research, education, humanitarian, and clinically-relevant materials contained therein, a growing WABIP Academy enriches membership with credible libraries of information, committees function functionally, leadership changes are transparent and bathed in dialogue, three representative scientific journals remain affordable and pertinent, our world congress and three regional meetings are almost overwhelming with useful information, Train-the-Trainer and other Bronchoscopy International educational programs positively influence physician-educators around the world, and our Whats App groups network more than 2000 physicians from thirty different countries in real-time.
Wow!
But what really impresses me is how our leadership strives to address, understand and nurture diversity. The new chair is a woman and a member of the Latin American bronchology community, thereby breaking an IP glass ceiling (prior chairs were men from Asia, Europe or the United States). The treasurer is an Australian and President of the next Asian Pacific meeting scheduled for March, 2019. The two next World Congress presidents are from China (2020) and France (2022), and our newly-elected Vice-Chair is a well-known opinion leader from Japan. Furthermore, Committee members and Committee chairs are selected using a democratic call for nominations and volunteers with special care to represent the global community, and the WABIP social media/Facebook presence is growing almost exponentially, and you can try this.
Hurrah!
I am proud of this association, and I encourage members to take an active role, not only in growing their regional and national bronchology/IP societies, but also in the WABIP. Collaboration and Cooperation are keys to our long-term success, which means greater equality among training programs regardless of their medical environment, more rapid dissemination of innovative technologies and techniques, more productive conversations with industry sponsors and equipment manufacturers, and most of all, greater steps forward in our efforts to help patients combat the effects of lung, airway, and pleural diseases.
Right on!



 While preparing yet another Train-the-Trainer program today, I came across this beautiful image that represents, for me, the beauty and wonder of teaching how to teach. After my morning exercises and thirty minutes of Zen meditation, I was thinking of which three “questions” to ask of the ten trainers who will join me at Olympus Headquarters in Melbourne, Australia later this evening for our working dinner. Usually, I open this session with an icebreaker exercise focused on active listening, followed by three interactive group exercises where each group tackles a challenging question such as “what is competency?”
While preparing yet another Train-the-Trainer program today, I came across this beautiful image that represents, for me, the beauty and wonder of teaching how to teach. After my morning exercises and thirty minutes of Zen meditation, I was thinking of which three “questions” to ask of the ten trainers who will join me at Olympus Headquarters in Melbourne, Australia later this evening for our working dinner. Usually, I open this session with an icebreaker exercise focused on active listening, followed by three interactive group exercises where each group tackles a challenging question such as “what is competency?”