I recently returned from a trip to Zion National Park, in the beautiful state of Utah, where a tragic accident led to the death of a 58-year-old man who fell while rappelling in Pine Creek Canyon. Known for its massive sandstone cliffs, giant slot canyons, and challenging hiking trails, the park is a famous destination for rock climbers and canyoneers alike. Just weeks earlier, in my home state of California, a 23-year-old experienced rock climber named Balin Miller made international news when he accidentally rappelled off the end of his rope after completing an ascent of the famous granite wall called El Capitan, in Yosemite National Park.
The problem with climbing accidents, whether from inattention, weather, climber and equipment error, or plain bad luck, is that they are unforgiving and often fatal. That is why so much attention is paid to accident prevention and to raising awareness about the risks of taking shortcuts or engaging, intentionally or unintentionally, in risky behavior. Miller, for example, was descending only a short distance to dislodge his equipment bag that had become stuck in a crack. He forgot or neglected to tie a knot in the end of his rope, ran out of line, and slid off the end to his death.
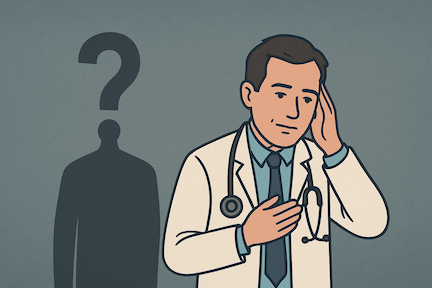
Accidents like this prompt me to think about the concept of risk normalization, also referred to as “normalization of deviance,” which describes how risky behaviors or operating in potentially dangerous conditions can become increasingly acceptable over time because of the absence of negative consequences. In other words, “repeated exposures to hazards without consequence lowers the perception of danger.” Think about texting while driving, bypassing infection control protocols, riding your motorbike without a helmet, or taking a casual approach to a risky activity.
For individuals, organizations, and society-at-large, any drift in behavior, cultural acceptance of potentially risky behaviors without appropriate safeguards, and reduced perception of hazards are all linked to risk normalization. I am amazed, for example, at the lingering resistance to using checklists to assure patient and procedure-related safety in interventional pulmonology. Also, I am intrigued by hundreds of videos of successful complex bronchoscopic interventions presented at national conferences or on WhatsApp, but very rarely is there a discussion of “close calls” or of something that went wrong.
Risk normalization is one of several invisible epidemics that threaten our overall well-being. It is fostered by complacency, desensitization, and an unwillingness, at times, to speak truth to power. It is a menace to professionalism that affects our ability, or reflects an unwillingness, to reason, and it represents a cultural drift away from vigilance and the ethos of safety and prevention. Health care environments, specifically in procedure-related aspects of healthcare delivery such as interventional pulmonology, are fertile settings for its development.
- https://www.sfgate.com/national-parks/article/yosemite-fatal-fall-el-capitan-climber-21098663.php. Accessed 10/27/2025.
- https://americanalpineclub.org/news/2025/6/17/2025-climbing-accident-trends-what-the-data-tells-us. Accessed 10/27/2025.
- Dr. Valerie Karr. https://americanalpineclub.org/news/2025/10/15/the-prescriptionground-fall. Accessed 10/27/2025.
- Nejc Sedlar N., Irwin A., Martin D., and Roberts R. A qualitative systematic review on the application of the normalization of deviance phenomenon within high-risk industries. Journal of Safety Research, Volume 84, 2023. Pages 290-305. https://doi.org/10.1016/j.jsr.2022.11.005.