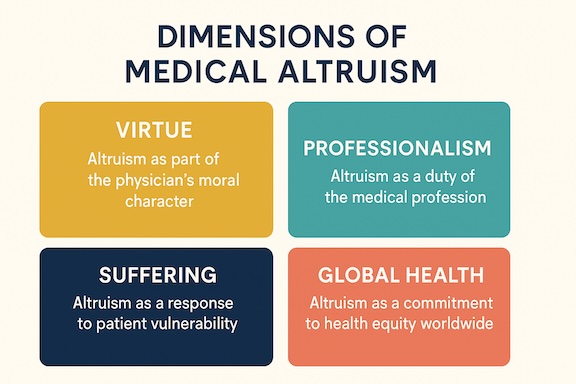
Medical altruism is usually considered a virtue that is critical to defining a physician’s moral character. However, one of its more noticeable manifestations is behavioral, reflecting compassion, responsibility, and a sense of moral obligation. Indeed, medical altruism translates into a commitment by health care providers to use their power, position, privilege, and knowledge in the best interests of others, even at great personal cost and varying degrees of effacement of self-interest. Therefore, medical altruism represents physicians’ spoken and often unspoken commitment to act selflessly for their patients’ well-being, regardless of potentially conflicting professional duties, even at the expense of personal gain, safety, or well-being.
American philosophers Pellegrino and Thomasma thus argued that beneficent altruism was morally obligatory for physicians, placing it at the root of a “virtuous” physician’s character. “No one can make the conscientious professional do what she thinks is not in the interests of the patient or client,” they write, and “The physician of character will…reliably be expected to exhibit the virtues of fidelity to trust and effacement of self-interest.”
Other manifestations of medical altruism might have their roots in a person’s psychological profile. In part, this is because medical altruism is almost always viewed as being individual-centered, and therefore, potentially at the core of a physician’s personal identity. For example, some physicians’ altruistic behaviors are linked to their heartfelt desire to relieve suffering. This is reflected by physician and bioethicist Eric Cassell’s (1928-2021) belief that “The relief of suffering and the cure of disease must be seen as twin obligations of a medical profession that is truly dedicated to the care of the sick.” Dr. Cassell viewed suffering as a primarily subjective experience, describing it as “the state of severe distress associated with events that threaten the intactness of the person.”
A slightly different perspective was presented by Daniel Sulmasy, who is well known for his writings about the connection between spirituality and medicine. He argued to reaffirm Sir William Osler’s declaration that medicine was a calling, not a business. Dr. Sulmasy is a physician and philosopher who once lived as a Franciscan friar. Focusing on a physician’s character, he suggests that altruism is a virtue easily threatened by a malfunctioning or flawed medico-industrial complex. He warns that unsound training environments and the stress/realities of day-to-day medical business practices can potentially erode altruistic ideals.
Richard and Sylvia Cruess argue that if medicine is a profession, then medical altruism is a professional duty. They believe altruism is at the core of the physician-patient contract and a centerpiece of the social contract between physicians and society: “Based on the literature, society’s expectations of medicine are the services of the healer, assured competence, altruistic service, morality and integrity, accountability, transparency, objective advice, and promotion of the public good.” According to this position, physicians have a professional obligation to engage in altruistic behaviors, the degrees of which can be hotly debated. Additionally, medical institutions and health care policies should promote and support altruism from a systems perspective because altruism is both expected and contractually anticipated by society-at-large.
This brief discussion of the various dimensions of medical altruism would be incomplete without acknowledging the work of recently defunct physician and anthropologist Paul Farmer (1959-2022). Dr. Farmer supported Article 25 of the Universal Declaration of Human Rights: “Everyone has the right to a standard of living adequate for the health and well-being of himself and his family, including food, clothing, housing, and medical care….” He expanded upon patient-focused boundaries of medical altruism by proposing that health care providers be individual caregivers but also advocates in the battle to overcome social inequalities.
- Pellegrino, ED and Thomasma DC. The virtues of medical practice. Oxford University Press, 1993.
- Cassell, E. J. 1982. “The Nature of Suffering and the Goals of Medicine.” N Engl J Med 306 (11): 639–45.
- Sulmasy, Daniel P. (1993). What’s so special about medicine? Theoretical Medicine and Bioethics 14 (1):379-380.
- Cruess SR. Professionalism and medicine’s social contract with society. Clin Orthop Relat Res. 2006 Aug; 449:170-6.
- Farmer, P. Pathologies of power: Health, human rights, and the new war on the poor. University of California Press, 2003.